
Connecting neurotransmitters, mood and eating disorders
Major depressive disorder is one of the most common mental health diagnosis to co-occur with eating disorders with between 50% to 75% of those that are living with an eating disorder also experiencing symptoms of depression. The bidirectional link between nutrition and emotions plays a critical role in determinate a persons overall health. In this blog I set out to help you understand what an eating disorder is, how neurotransmitters work and the connection between the two.
What is an eating disorder?
Eating disorder are behavioural conditions characterized by severe persistent disturbance in eating behaviours and associated distressing thoughts and emotions.
Eating disorders are often associated with preoccupation with food, weight and shape, or anxiety about eating or the consequences of eating certain food.
According with the National eating disorder Collaboration approximately one million Australian are living with an eating disorder in any given years.
Of people with eating disorder, 3% have anorexia nervosa, 12% bulimia nervosa, 47% binge eating disorder (BED) and 38% other eating disorders.
Three main type of eating disorders
Anorexia nervosa
That occurs when a person refuses to eat an adequate amount of food or is unable to maintain a minimally healthy weight (BMI below 18.5) .
Individual with anorexia often have a distorted body image, and they typically engage in severely restricting food intake, often compulsive exercise or abuse of laxative, enemas and diuretics.
Bulimia nervosa
Is characterised by episodes of binge eating, consuming a large amount of food, followed by compensatory behaviour such as vomiting or the abuse of diuretics or laxative.
They often feel a lack of control over their behaviour. They typically know they have a problem yet often fear they are unable to stop engaging in binges, leading them to engage in purging behaviours to avoid weight gain.
Binge eating disorder (BED)
Involves the recurrent consumption of a large amount of food in a short amount of time. Binge eating episodes are associated with eating more rapidly than normal, eating until uncomfortably full, eating large amounts of food when not physically hungry, and feeling disgusted with oneself or depressed afterwards.
What is the cause of an eating disorder?
Eating disorder often co-occur with other psychiatric disorders most commonly mood and anxiety disorder, obsessive compulsive disorder and alcohol and drugs abuse problems.
Evidence suggest that genes and heritability play a part in why some people are at higher risk for an eating disorder, but these disorders, can be afflict from trauma.
Eating disorders are serious, complex and potentially life threatening mental illness.
There are three basic pillars for development of eating disorders, according to the psychiatric Semra Bozkurt Zincir, genetic predisposition, neuroendocrine- molecular changes in the brain and metabolic response to it.
Understanding Neurotransmitters
While hundreds of neurotransmitters have been identified thus far by science, there are three in particular that have been studied extensively and found to strongly influence emotion and behaviour:
- Serotonin
- Dopamine
- Norepinephrine.
Those chemicals are closely tied to appetite, mood, and impulse control, which has been shown to be altered in people with eating disordered.
Dopamine
It is a neurotransmitter made in a brain. It plays a role in many body functions, including memory, movement, motivation, mood, attention and pleasure. Dopamine is known as the “feel good” hormone. It gives you a sense of pleasure, it is part of your “reward system”, this system is designed, from an evolutionary standpoint, to reward you when you are doing the things you need to do to survive, such as eat, drink, and reproduce. As human, our brain are hard-wired to seek out behaviours that release dopamine in our rewards system.
When you are doing something pleasurable, your brain releases a large amount of dopamine. You feel good and seek more of that feeling.
This the reason why recreational drugs, alcohol, sugar and at some stage food, especially junk food can be so addictive.
Serotonin
Serotonin is another chemical that carries messages between nerve cells in the brain and through your body. It plays a key role in such body function as mood. Sleep digestion nausea, sexual desire, and appetite.
Norepinephrine
Norepinephrine, also call noradrenaline, is released predominantly from the ends of the sympathetic nerve fibres. The actions of norepinephrine are vital in response to stress and threat or what we call the “fight- and – flight responses.
Norepinephrine plays a role motivation and concentration.
The link between neurotransmitters and eating disorders
Although eating disorders result from the interplay of a variety of cultural and biological factors, the brain is central to understanding why some people develop eating disorders, why people stay ill, and how they can recover.
For instance, alteration in brain serotonin function are though to contribute to diverse aspects of eating disorders, including beige eating, perfectionism, impulsivity and mood regulation problems. in
The vicious cycle
Research has shown that there is a relationship between certain personality, genetic, temperament and vulnerability to eating disorders. Anxiety, perfectionism, and obsessive traits can make an individual vulnerable to managing life stressors through problematic eating. In the other hand, chronic use of restrictive eating and binge- purging leads to neurobiological and pathological changes in body functions, such as changes in the microbiome diversity and health, (which they are well known to be linked to mood regulation and serotonin production, as well as Gut and immunity health), hormonal dysregulation, increase of stress level, and decrease immune function and energy.
Those changes in the body could increase denial, rigidity, depression, as well as anxiety and perfectionism. With the increase of this symptoms the individual is yet again more vulnerable to relying on problematic eating to manage these feelings.
How can a naturopath help?
A naturopath may be an essential member of a multidisciplinary clinical team to treat a patient holistically.
Eating disorders are complex and multifaceted, while sometimes a medical approached is needed, especially in severe cases of starvation, the most common treatment involved a health care team to help the patient recover from an eating disorder. This team may include a psychologist, psychiatric or counselor, nutritionist, naturopath or dietitian, as well as support groups.
Usually, a professional health care team works in collaboration for support the both physical and psychological aspect of the disorders.
A naturopaths approach may include:
Genetic testing
Eating disorders can be associated a genetic component or ‘predisposition’ and the possibility of brain chemical disfunction. Functional genetic testing can give a better into the genetics of the patient and can help us to better understand the root cause of the disorder.
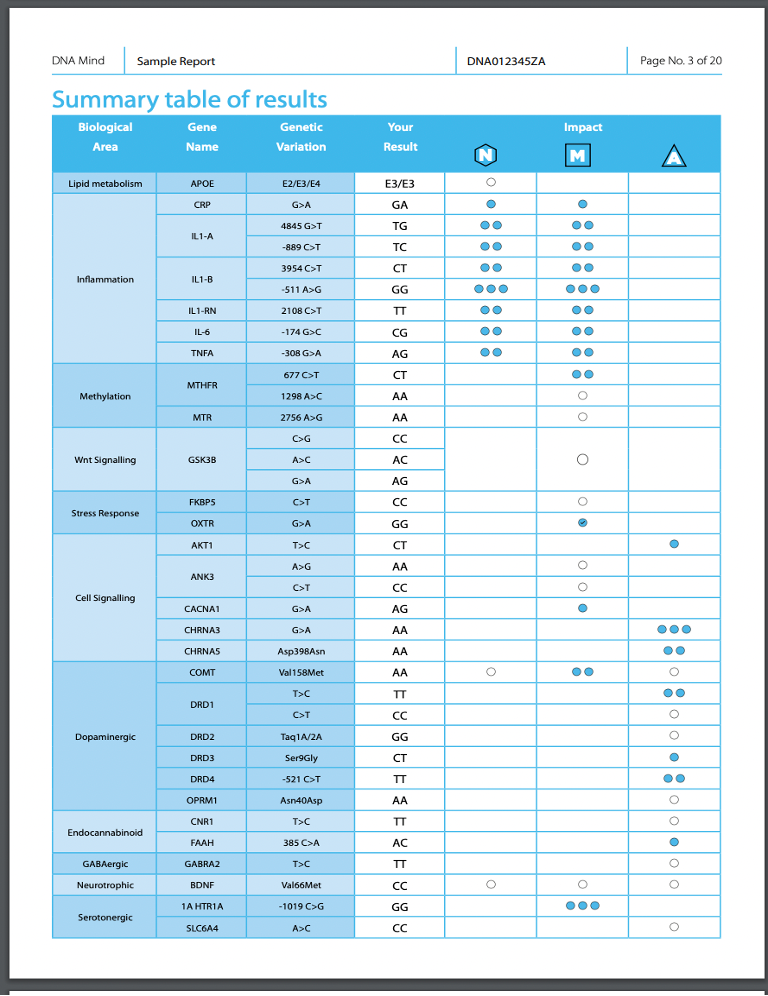
This is a sample of DNA Mind from RN labs company, it analyses 30 genes which have been shown to have significant associations with key mental health disorders.
Food as medicine
Perhaps one of the most important steps in recovery from eating disorders is nourishing and feeding the body, but it is also one of the harder challenges for individuals that experience these disorders.
Refuelling a body with adequate nutrition is crucial for overcoming the stronghold of eating disorders.
When an individual with an eating disorders drastically reduces their nutrients intake, the little that they eat is used only for the most vital bodily processes. Non-essential biological functions, on the other hand, begin to be shut down by the body itself.
Hormones production slows, and susceptibility to infections are common, hair and nails can become brittle and breaking easily.
Eventually, even essential functions, including those that regulate the activity of the heart, became alert, this is why reintroduce a correct diet is essential for the treatment of an eating disorders.
The naturopath role is to help a patient make healthy eating part of their everyday life, educate the patients on having a stress- free relationship with food and she will plan a tailored diet, to make sure the patient get al the essential proteins, carbohydrates, fats, vitamins and mineral the body needs.
Amino acid therapy
Protein is necessary when treating disorders that have a link with mood, protein are made from amino acid, and those are precursor of neurotransmitters.
Due to the luck of nutrients that come with the eating disorders, supplementation with single and specific amino acid will help regulate the production of neurotransmitters and consequently helped with decrease symptoms such as depression, anxiety, focus and perfectionism.
As already mentioned, the main neurotransmitters that have been link with emotional behaviours are serotonin, dopamine, and norepinephrine, all three are constructed from amino acid precursors obtained from the diet.
The precursor of serotonin is tryptophan, while the precursors for dopamine and norepinephrine can be the amino acids phenylamine and tyrosine.
Most neurotransmitters are under precursor control, which means that not eating specific amino acid will result in depleted amounts of the related neurotransmitters in the brain.
A study in Germany shown that both subject with weight- recovered and actually ill subject with anorexia nervosa has significantly lower level of tryptophan and phenylamine that did the healthy control group.
Support GUT and reduce inflammation
The GUT and GUT microbiome has been shown that has a direct link with the brain and the production of neurotransmitters.
Reduce Gut inflammation and replenish an healthy microbiome colony will help with symptoms of anxiety and depression as well as increase nutrients absorption
Check this amazing Blog of Brooke Shiller for a better understanding of the gut brain connection and how you can improve it.
Herbal medicine
Botanical medicine will help on different aspects.
Herbs such Gentian, Ginger, dandelion root, angelica root, globe artichoke are consider to be bitters herbs.
For individual in recovery from an eating disorder, the task of reintroducing the food we should become more difficult when faced with digest upset, those type of herbal medicine have the effect of increase digestive function, and they are specifically used to increase digestion, and help in the process of healing by facilitate nutrients breakdown and absorption.
Herbs such as Kava, lavender, lemon balm, and ashwagandha could help with anxiety symptoms, while herbs such St john’s wort, lavender, skullcap could help with symptoms of depression.
Both depression and depression and anxiety are commonly present in patients with eating disorders, reducing anxiety and depression symptoms is an important part of the treatment , a clear state of mind will make the journey of engaging in healthy habits easier.
Make sure you approach a health practitioner before star taking any supplements or herbal medicine.
Recovering from an eating disorder can seem a dauting process and understanding the foundations of your recovery can be instrumental in making forwards progress. If you or a loved one has struggled to take that first step, know that you are not alone in this process, if you want some support or more clarification on how to start your recovery journey, please get in touch and booking in a Base or a Simplify Section Here.
Liked this article, want to learn more.
Related posts
Natural treatments for dysbiosis
Our vaginal microbiome plays a crucial role in overall vaginal he
Fuelling The Vaginal Microbiome Blog
What is the vaginal microbiome? Much like the gut, the vagina has





