
Everything you need to know about Perimenopause & Beyond
Have you started noticing changes to your periods? Are they becoming longer and heavier? Are your moods more varied in the way you respond to your kids or partner? If you are over 35 years old there is a chance your body is getting ready for its ‘second puberty’ which we know to be perimenopause.
What is perimenopause?
Perimenopause refers to the time in a woman’s life before menopause (the final menstrual period). Typically perimenopause will start in our 40’s (or possibly late 30’s) where the body will produce less progesterone (even if you are still having regular periods). It is the lowering of this hormone which is linked with so many of the symptoms we experience during this stage;
- Irritable mood
- Breast pain
- Heavy periods
- Pelvic pain
- Migraines
- Night sweats
- Anxiety
- Depression
It is the changes in oestrogen later in perimenopause that you might experience insomnia, memory loss, vaginal dryness, and insulin sensitivity (which is a major contributor to abdominal weight gain).
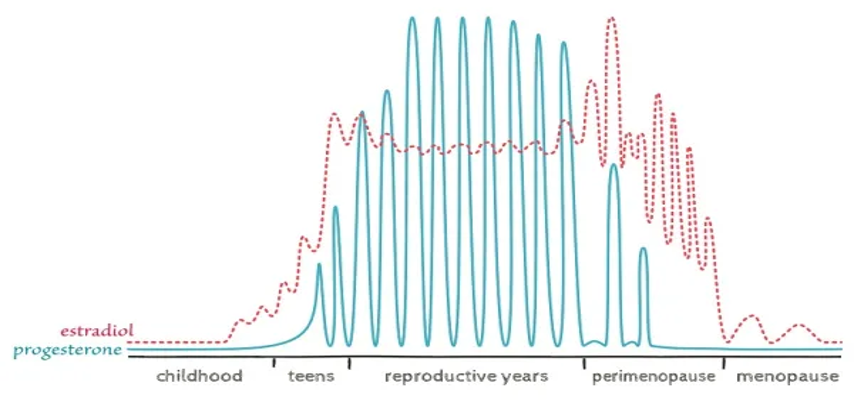
During perimenopause you are likely to follow this sequence of events:
- Lower progesterone
- High and fluctuating oestrogen
- Lower oestrogen
- Possible insulin resistance
Can you test for Perimenopause?
Generally your GP won’t run hormone tests during their perimenopause years due to the fluctuation in oestrogen and progesterone. You can have your FSH hormone checked as a marker to see if you are in early peri, or late per. FSH (follicle stimulating hormone) is released from your pituitary gland and communicates to your ovaries. If you are not yet in Menopause your FSH level will be <40. Clinically we use detailed information gathering to determine if you are in perimenopause by classifying many of the signs and symptoms, alongside with your age and family history.
The stigma around Perimenopause and Menopause
This is a real experience many women will feel and may even believe. The idea that menopause is only linked with women in their 60’s is not an true or accurate. The fact is we as women need to speak openly about our hormonal health, so these issues can become part of the mainstream conversation of women’s health.
The National Institute in Health (NIH) has a historical lack of data focusing on testing women and women’s health concerns which has compromised women’s health care. Until 1993 women weren’t included in clinical trials due to women’s hormonal variables.
In Australia there are no formal regulations to pass a regulation/rule stating we need to include women in research studies.
What will affect my symptoms during Perimenopause?
Genetics
This will determine both the timing of menopause and severity of symptoms (to some degree). Even though they give a glimpse of what it might be like. We now know that gene health can be affected positively and negatively by nutrition, environment, and circadian rhythms (sleep).
General Health
Perimenopause can be like a predicter of your overall health. If you are already stressed, not sleeping well, and deficient in iodine, zinc, and magnesium the ups and downs of oestrogen could make perimenopause a very unpleasant experience for you.
If you are already at risk of insulin resistance (poor sleep, high carbohydrate diet, low level physical exercise, and high alcohol intake) the shift to lower oestrogen could push you into full insulin resistance and abdominal weight gain.
Period health pre- perimenopause
If you had easy periods, you are more likely to experience and easy perimenopause. As symptoms free periods are a good indicator that everything is working well (including the clearance of oestrogen metabolites).
If you have had more difficult periods, you may experience a more difficult perimenopause as the same things which effect your menstrual cycle are likely to effect your perimenopause.
What can we do to support the body through Perimenopause?
Supporting your autonomic and parasympathetic nervous systems
Calm the Vagus nerve by:
- Getting outside into nature
- Building social connections
- Breathing techniques with long exhalations (yoga)
You can read more on the Vagus Nerve on Margarets great blog here.
Regulate circadian rhythms
- Morning and evening light- blue waves light in the morning, blue blocking light at night. Morning protein 10gm by 10am
- Reduce alcohol (see notes below)
- Melatonin- speak to your GP about possibly prescribing this
Reduce inflammation
- Assess and address underlying chronic inflammation; autoimmune, gut dysbiosis, underlying hormonal issues like endo, fibroids, PCOS.
Treat Insulin resistance
- Abdominal weight gain is the major sign of insulin resistance. A waistline measurement above 89cm will indicate abdominal fat tissue linked with some level of insulin resistance.
- To test insulin resistance: have a GGT with fasting insulin.
- Gluten and dairy free diets can be helpful with the use of intermittent fasting, under the right circumstances.
Diet for perimenopause
Protein intake
Adequate protein intake is essential for building muscle, and regulating insulin. Two key points in perimenopause are to build muscle and regulate insulin. 20-25gm protein 3 times daily. If you are vegan or vegetarian there are a variety of supplements you can use to provide your body with enough vitamins, amino acids and minerals.
Fat and carbohydrate intake can vary depending on the individuals needs, but protein needs to stay stable in every woman’s diet.
Phytonutrients (naturally occurring plant chemicals)
- Polyphenols– purple foods, spinach, pecans, almonds, walnuts, potatoes, onions, broccoli, asparagus, berries, pomegranates, plums, dark chocolate, herbs and spices.
- Flavonoids– capsicum, kale, broccoli, spinach, red cabbage, parsley, tea, grapefruit, lemon, soy beans
- Lutein– green leafy vegetables, kale, broccoli, spinach, beans, peas, lettuces, egg yolks, pumpkin, carrot, pistaccios
- Resveratrol– grapes, peanuts, blueberries, cranberries, pistaccios,
- Sulfurophane- cruciferous veggies, activates Nrf2 which activates hundreds of detoxifying genes. Broccoli, kale, cauliflower, brussel sprouts, cabbage, bok choy, sprouts.
Phytoestrogens (plant oestrogens)
These occur naturally in almost all plant foods. They come in the form of iso-flavones (from soy) and lignans (from seeds + whole grains, legumes, fruits and veg).
They interact with oestrogen receptors but they are not oestrogen. They bind weakly and block oestrogen from binding- which is why during the later stages of perimenopause when you have 3 times higher amounts of oestrogen circulating your body, blocking some of these sites with phytoestrogens can help regulate symptoms such as hot flushes and heavy periods.
Avoid snacking
This increases insulin, and puts stress on the immune and digestive systems. If you are struggling to reach the 20gm protein goal then use a snack to help elevate this such as a collagen smoothie, 2 eggs on paleo toast, handful of walnuts and beef jerky, pate on seeded crackers. However if you are managing to get your regular 3 meals per day and a 2 serves of fruit you may not need additional snacks.
Which nutrients and Herbs are best during perimenopause?
This will depend entirely on your experience and your symptoms. The three most important nutrients to start with are:
- Magnesium (safe to supplement)
- Zinc (assess dietary intake)
- Iodine (test first)
And then from there depending on your symptoms you can see which herbs or nutrients may help support you best. We can support you in our clinic for tailored advice on your unique presentation and sourcing good quality products that contain the below.
| Symptom | Nutrient | Herb |
| Anxiety + Irritability | Magnesium 300-400mg daily Taurine 3gm daily Vitamin B6 30mg twice daily SAM-e 200mg daily | St John’s wort Zizyphus Passionflower Withania Chaste tree |
| Breast Pain | Iodine (test first) >150mcg usually required Evening primrose oil > 3gm daily Calcium-d-glucarate 1000-1500mg daily | Chaste tree Blue Cohosh Ginkgo Calendula |
| Heavy Periods + Pelvic Pain | Magnesium 300-400mg daily Vitamin B6 30mg twice daily Omega 3 EPA/DHA 3gm twice daily Iron bisglycinate (test first) 25mg daily Zinc glycinate 25mg daily Iodine (test first) >150mcg Calcium-d-glucarate 1000-1500mg daily | Turmeric Chaste tree California poppy Cramp bark Black Cohosh Dong Qaui Ginger Fennel Wild Yam Raspberry leaf |
| Hot flushes | Magnesium 300-400mg daily Taurine 3gm daily | Black Cohosh Sage Motherwort St Johns wort |
| Disrupted sleep | Magnesium 400mg taken 2 hours before bed Glycine 3-5gm 1 hour before bed Taurine 3gm 2 hours before bed | Zizyphus Magnolia Passionflower Lavender |
| Migraines | Magnesium glycinate 300mg twice daily Vitamin B2 200mg twice daily Iron bisglycinate (test first) >20mg | Feverfew Jamaica Dogwood Willow Bark Peony Lime flowers Valerian |
| Memory Loss | Omega 3 EPA/DHA 3gm twice daily Vitamin B12 1000mcg daily Choline 500mg daily | Bacopa Ginkgo Green tea Rhodiola |
| Vaginal Dryness | Lactobacillus crispatus Lactobacillus acidophilus Probiotics Omega 3 3gm twice daily Vitamin A 5000-6000IU | Wild Yam Tribulus False unicorn root |
| Insulin resistance | Inositol 2gm twice daily Chromium 25ug twice daily Magnesium bisglycinate 200mg twice daily | Cinnamon Gymnema Bearberry Golden seal |
Exercise
Sarcopenia is something experienced by most woman after menopause, and for some during perimenopause. It refers to the loss of muscle tissue. This is one area you have a good level of control over preventing its loss. By increasing weight based exercise in the form of strength and weight training you can increase your muscle mass and promote cellular energy. This isone area your body will thrive at this stage in your life and respond really well to the type of exercise.
Yoga, pilates, swimming, hiking, walking, running are all beneficial in many other ways, but “Lifting Heavy” is one way you can train your body to retain muscle and bone mass and prevent osteoperosis, insulin resistance, and prevent excess weight gain.
Perimenopause is something which happens to every woman during her lifespan. It is normal and natural and doesn’t need to be interfered with in many cases. Knowing your body and how you can support it with nutrition and lifestyle can be empowering and reassuring. Always check in with your medical practitioner if you feel there are changes taking place which concern you and know that Naturopathy offers a modality which is complimentary to your needs at this stage.
Author
Claire Gruellemans
Naturopath BhSc
Claire is a senior naturopath with a focus on women’s hormonal health throughout the lifespan.
Learn more about Claire here
Book a session with Claire here
References:
Lara Briden “Hormone repair Manual” 2021
Ruth Trickey “Women, hormones, and the menstrual cycle” 2003
Kerry Bone “The ultimate herbal compendium” 2007
Kira Sutherland “Perimenopause and beyond webinar by Vital.ly” 2023
Professor JC Prior “Perimenopause lost- reframing the end of menstruation” Journal of reproductive and infant psychology 2006





