Your Guide to Lowering Insulin Levels
Insulin resistance is a condition we see often at Hälsa Health. It’s a key feature in polycystic ovary syndrome (PCOS) and weight presentations, and is a metabolic block to people reaching their weight and hormone balancing goals.
WHAT IS INSULIN?
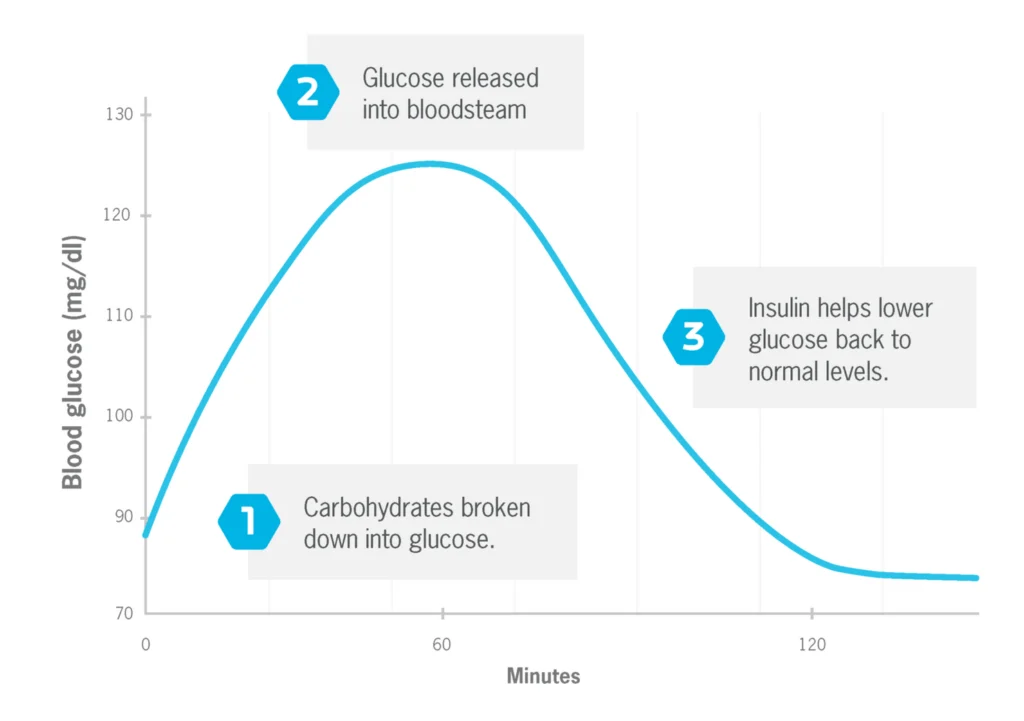
Insulin is a hormone made by the pancreas that helps to move glucose from your blood into your liver, muscle and fat cells, where it’s used for energy. After we eat, food is broken down into glucose and transported in the blood. When blood glucose levels rise after eating, your pancreas releases insulin, which then lowers blood glucose by moving the glucose into your cells. This helps to keep blood glucose (aka blood sugar) levels stable and in a normal range.
WHAT IS INSULIN RESISTANCE?
Insulin resistance is when your cells don’t respond well to insulin and can’t easily up-take glucose from your blood. To combat this, your pancreas makes more insulin to help move glucose into your cells. Your blood glucose levels will stay in the healthy range if your pancreas can make enough insulin to counteract the weak response from your cells to insulin. If your pancreas cannot keep up your blood glucose levels become high, which overtime can lead to prediabetes.
Insulin resistance primarily occurs due to excess body fat (especially around the abdomen), although genetic causes are identified as well, as people with lean PCOS will attest to.
SIGNS OF INSULIN RESISTANCE
- Sugar cravings
- Extreme thirst
- Insatiable appetite
- Low energy levels
- Frequent urination
- Weight gain, or being unable to lose weight
HOW TO TEST FOR INSULIN RESISTANCE
See your health practitioner and request a fasting insulin test. The optimum target range is between 4-6 mU/L.
You may like to complete fasting glucose, HbA1c, and glucose tolerance testing at the same time, as all are related to blood sugar levels.
Fasting means that you need to abstain from food for 8-10 hours (generally overnight), and get the test done in the morning. Water is fine to have while fasting.
RISK FACTORS FOR INSULIN RESISTANCE
- Western style diet (high in processed carbohydrates & sugars)
- Being overweight
- Sedentary or inactive lifestyle
- PCOS (high insulin is both a symptom of PCOS and an underlying physiological driver)
- Diabetes, cardiovascular disease, nonalcoholic fatty liver disease, metabolic syndrome, or a family history of the aforementioned conditions
HOW TO REVERSE INSULIN RESISTANCE
DIETARY ADJUSTMENTS
Dietary adjustments are the most effective way to reduce insulin resistance! Start with the following:
- Consume a diet of fresh fruit & vegetables, complex carbohydrates, fibre, lean protein and healthy fats
- Avoid or go low sugar. Fresh fruit is fine, aiming for < 25g fructose per day
- Avoid simple carbohydrates such as white bread, white pasta, white rice, biscuits, cakes, pizza, burgers, chips and soft-drinks
- Avoid trans-fats, deep-fried foods and oxidised fats (rancid oils, smoked oils)
- Revisit your portion sizes
- Consider the glycemic index of foods
EXERCISE
Exercise helps by improving insulin sensitivity in muscles. Find movement that you enjoy and aim for 30 minutes 5 days per week. HIIT training is thought to be especially beneficial, but is not appropriate in the case of high stress levels.
EATING WINDOW
Time restricted eating improves blood glucose and insulin sensitivity. Experiment with a 10 hour window of when you consume food, for example eating breakfast at 9am and finishing dinner by 7pm.
MAGNESIUM
Magnesium is a key nutrient prescribed in insulin resistance, as deficiency impairs insulin secretion. Increase your consumption of leafy green vegetables, whole grains and nuts. When supplementing, I recommend magnesium bisglycinate 200mg twice daily after food.
VITAMIN D
Vitamin D deficiency has been shown to be correlated to insulin resistance. Maintenance levels of Vitamin D can be achieved by 20 minutes of sunshine on bare skin three times weekly. This is a worthy marker to test, to ensure levels are optimum. The goal is > 70 nmol/L in Winter and > 100 nmol/L in Summer. Supplementation depends on what your levels are to start with. If sunshine levels are inadequate, a maintenance dose of 1000IU per day is recommended.
CHROMIUM
Chromium is required for the uptake of insulin into the cells, and can help to reduce sugar cravings. Dietary sources include egg yolks, beef and shellfish. If supplementing, try 200mg twice daily after food.
INOSITOL
Inositol is an intracellular messenger involved in insulin signalling. The recommended dose for supplementation is 2g twice daily with food. Dosing can go higher than this if needed, so be guided by your practitioner. Inositol is also highly indicated if your insulin resistance is part of PCOS.
ALPHA LIPOIC ACID
Alpha-lipoic acid works by enhancing the uptake of glucose that is initiated by insulin. If supplementing I suggest 300-600mg per day with food.
RESVERATROL
Resveratrol is an antioxidant that improves insulin signalling. It’s found in blueberries, pistachios, cocoa and red wine, although the researched dose is far greater than you could consume from food sources. Recommended dose for supplementation is 200mg daily.
HERBAL MEDICINE
There are a number of herbal options effective in lowering insulin levels, such as goats rue, gymnema, fenugreek, cinnamon, ginseng, bitter melon, garlic, curcumin, ginger, and berberine. I recommend using herbs under the guidance of a practitioner.
She Glows is a lovely tea to support inulin resistance as it contains cinnamon and is helpful in reducing sugar cravings.
Fun fact – Goat’s Rue contains an active compound called galegine. Modern studies of galegine led to the creation of metformin, which is a medication used to lower insulin levels.
REFERENCES
https://www.ncbi.nlm.nih.gov/books/NBK507839/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1204764/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6587894/
https://www.imrpress.com/journal/FBE/7/1/10.2741/E720
https://link.springer.com/chapter/10.1007/978-3-030-64872-5_13
https://www.frontiersin.org/articles/10.3389/fphar.2019.00661/fullhttps://nutritionandmetabolism.biomedcentral.com/articles/10.1186/s12986-021-00613-9
If you are experiencing insulin resistance symptoms and would like individualised support, please get in touch by booking in a Base Chat or Simplify Session here.
Brooke is a qualified naturopath with a focus on digestive health, hormones, and adrenal conditions.
Liked this article, want to learn more
Book in a free base chat with our practitioners to understand the best diet & lifestyle shifts, herbal or nutritional options for you. All of our practitioners are clinically trained and evidence based registered with Australia’s leading associations.
Follow up on Instagram for more tips, support and fun here
Tags:
Insuline ResistanceRelated posts
Natural treatments for dysbiosis
Our vaginal microbiome plays a crucial role in overall vaginal he
Fuelling The Vaginal Microbiome Blog
What is the vaginal microbiome? Much like the gut, the vagina has